When taking care of your prostate, knowing about the tests is essential. One test that’s getting attention is called a Transperineal Prostate Biopsy. This article goes deep into what this test is about – how it’s done, why it’s good, what might happen after, and how you recover. We’re here to explain it all, so if you’re facing this choice, you can make a decision knowing all the details. Let’s get into “What Is a Transperineal Prostate Biopsy?” and understand it better.
1. What Is a Transperineal Prostate Biopsy?
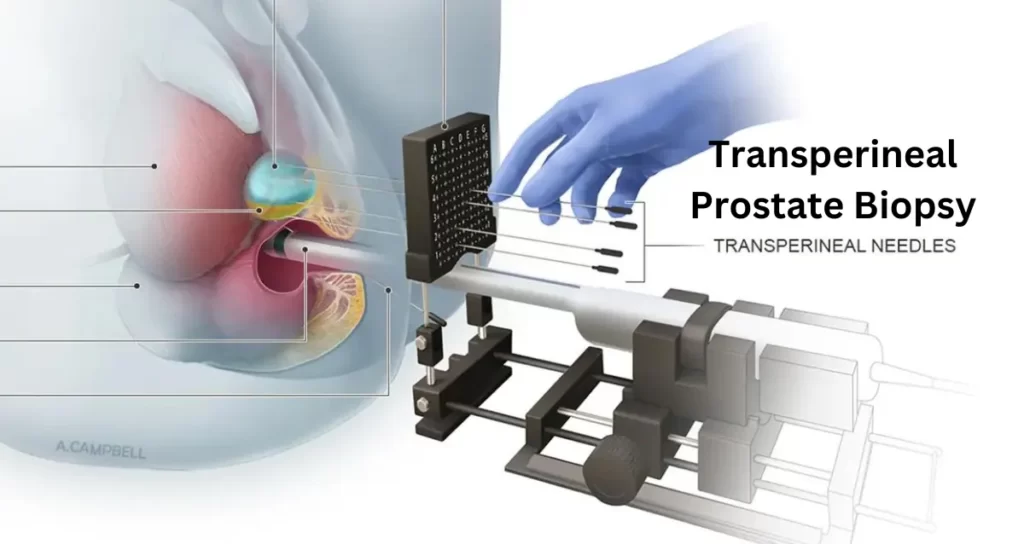
At its core, a transperineal prostate biopsy is a diagnostic procedure aimed at assessing prostate health. Unlike other biopsy methods, this technique involves accessing the prostate through the perineum, the area between the scrotum and anus. This unique approach allows for targeted sampling of prostate tissues.
What is the Breast Cancer Index Test? A Gateway to Timely Detection.
2. Step-by-Step Transperineal Prostate Biopsy Procedure
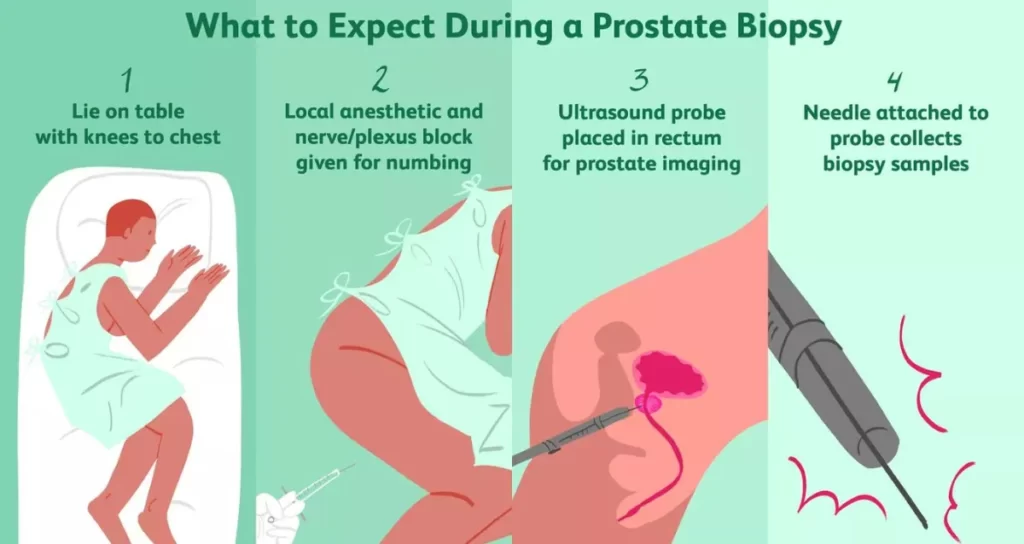
A transperineal prostate biopsy is a diagnostic procedure designed to assess the health of the prostate gland. Here’s a detailed, step-by-step explanation of the process:
Step 1: Patient Preparation
Before the procedure, the patient will be informed about the biopsy, its purpose, and any necessary preparations. This may include discontinuing certain medications or dietary restrictions.
Step 2: Anesthesia Administration
To ensure the patient’s comfort, local or general anesthesia is administered. The choice of anesthesia depends on the patient’s health, preferences, and the medical team’s recommendation.
Step 3: Positioning
The patient is positioned on their back, with legs elevated or bent at the knees. This exposes the perineum, the area between the scrotum and anus, for easy access to the prostate.
Step 4: Sterilization
The perineal area is thoroughly cleaned and sterilized to minimize the risk of infection during the biopsy.
Step 5: Ultrasound Guidance
Using transrectal or transperineal ultrasound, the healthcare professional locate the prostate gland. Transperineal ultrasound involves placing a probe on the perineum, providing precise imaging of the prostate’s size, shape, and any abnormalities.
Step 6: Biopsy Needle Insertion
A biopsy needle is then guided through the perineum, entering the prostate gland to collect tissue samples. The medical professional carefully maneuvers the needle to target specific areas of interest.
Step 7: Tissue Sample Collection
Multiple tissue samples are collected from different prostate regions with the needle in position. This comprehensive approach ensures a thorough examination of the gland.
Step 8: Hemostasis
After obtaining the necessary samples, the healthcare provider ensures no excessive bleeding by applying gentle pressure or specialized techniques.
Step 9: Post-Biopsy Care
Once the procedure is complete, the patient is monitored for a short period. Post-biopsy care instructions are provided, including any prescribed medications or activity restrictions.
Step 10: Monitoring and Follow-Up
The patient’s recovery is monitored, and immediate concerns or complications are addressed. Follow-up appointments are scheduled to discuss biopsy results and plan further treatment if necessary.
It’s important to note that the success and safety of a transperineal prostate biopsy depend on the expertise of the healthcare professionals performing the procedure. Patients are encouraged to communicate openly with their medical team, addressing any concerns or questions about the biopsy process.
3. Advantages of Transperineal Prostate Biopsy
A transrectal prostate biopsy offers several advantages compared to alternative biopsy methods. Understanding these benefits is crucial for individuals making decisions about their prostate health. Here are the key advantages:
1. Lower Infection Risk: One significant advantage of the transperineal approach is the lower risk of infection. By accessing the prostate through the perineum, which is less susceptible to bacterial contamination compared to the rectum, the chances of post-biopsy infections are significantly reduced.
2. Enhanced Accuracy: The transperineal biopsy method allows for enhanced accuracy in targeting specific areas of the prostate. This precision is vital for obtaining accurate diagnostic information, ensuring the biopsy effectively identifies abnormalities or concerns within the gland.
3. Comprehensive Tissue Sampling: The procedure allows for comprehensive tissue sampling from various regions of the prostate. This extensive sampling thoroughly assesses the gland’s health, aiding in a more accurate diagnosis and a better understanding of the patient’s condition.
4. Reduced Risk of Rectal Injury: Unlike transrectal biopsy methods, which involve passing the biopsy needle through the rectal wall, transperineal biopsy reduces the risk of rectal injury. This contributes to a safer procedure with fewer potential complications.
5. Improved Patient Comfort: Patients often report greater comfort with the transperineal approach. Avoiding the rectum in the biopsy process can reduce discomfort during and after the procedure, contributing to an overall more positive patient experience.
6. Minimized Procedural Discomfort: With local or general anesthesia guidance, patients experience minimized procedural discomfort during a transperineal biopsy. This ensures that individuals undergoing the biopsy are as comfortable as possible.
7. Adaptability for Repeat Biopsies: In cases where repeat biopsies are necessary, the transperineal approach remains viable. It allows for repeated sampling without the heightened risk of infection associated with multiple transrectal biopsies.
8. Suitability for Individuals with Rectal Conditions: For individuals with pre-existing rectal conditions or those who have undergone rectal surgery, transperineal biopsy provides a suitable alternative. It avoids potential complications related to the rectum, making it a safer option for these patients.
Understanding these advantages empowers individuals and healthcare professionals to make informed decisions about the most appropriate biopsy method based on the patient’s unique circumstances and medical history. The transperineal prostate biopsy‘s combination of precision, safety, and patient comfort makes it a compelling choice in the realm of prostate health diagnostics.
4. Transperineal prostate biopsy Side Effects and Risks
While a transperineal prostate biopsy is a valuable diagnostic tool for assessing prostate health, it is essential to be aware of potential side effects and risks associated with the procedure. Understanding these aspects helps individuals make informed decisions about their healthcare. Here are the common side effects and risks:
1. Discomfort and Pain: It’s not uncommon to experience discomfort or mild pain in the perineal area during and after the biopsy. This is typically temporary and can be managed with prescribed pain medications or over-the-counter pain relievers.
2. Bleeding: A degree of bleeding is expected after the biopsy due to the needle punctures in the prostate. Patients may notice blood in their urine, stool, or semen. This is usually minimal and resolves within a few days. If bleeding persists or becomes severe, medical attention should be sought.
3. Infection: While the transperineal approach reduces the risk of infection compared to transrectal biopsy, there is still a tiny chance of infection. Patients are prescribed antibiotics before the procedure to minimize this risk. Any signs of infection, such as fever or increased pain, should be promptly reported to healthcare providers.
4. Urinary Difficulties: Some individuals may experience temporary urinary difficulties following the biopsy. This can include a slow urine stream, discomfort during urination, or blood in the urine. These issues are resolved independently, but persistent symptoms should be discussed with healthcare professionals.
5. Rectal Symptoms: As the procedure involves the perineum, there may be temporary rectal symptoms such as mild bleeding or discomfort. These symptoms are usually short-lived but should be communicated to the healthcare team.
6. Allergic Reactions: Though rare, individuals may have allergic reactions to medications or materials used during the biopsy. Allergies to local anesthetics or antibiotics can manifest as itching, rash, or difficulty breathing. Any allergic reactions should be reported immediately.
7. Rare Complications: In rare instances, more severe complications can occur, such as damage to nearby structures or organs. However, the likelihood of these complications is minimal, and healthcare professionals take precautionary measures to minimize such risks.
8. Psychological Impact: Undergoing a biopsy can be emotionally challenging for some individuals. Anxiety or stress related to the procedure is a valid concern. Healthcare providers must offer support and address any psychological impact on the patient.
9. Delayed Results: While not a direct side effect of the procedure, the time it takes to receive biopsy results can be challenging for patients. Waiting for results can cause anxiety. Healthcare providers should provide clear timelines for result delivery and be available to address patient concerns.
Individuals considering a transperineal prostate biopsy should discuss potential side effects and risks with their healthcare provider. Open communication ensures that patients are well-prepared for the procedure and can address any concerns or complications promptly.
5. After the Transperineal Prostate Biopsy

After undergoing a transperineal prostate biopsy, individuals can expect a period of recovery and monitoring. While the procedure is relatively straightforward, proper post-biopsy care is crucial to ensure a smooth and complication-free recovery. Here’s a guide on what to expect and how to navigate the post-biopsy phase:
1. Immediate Post-Biopsy Monitoring: Following the biopsy, individuals are typically monitored for a short period in a recovery area. This allows healthcare professionals to observe for any immediate complications or reactions to the procedure.
2. Pain Management: It’s normal to experience some discomfort or mild pain after the biopsy. Healthcare providers may prescribe pain medications or recommend over-the-counter pain relievers to manage any post-procedural pain. Following the prescribed dosage and informing the medical team of any severe or persistent pain is essential.
3. Bleeding and Discharge: Some bleeding is expected after the biopsy due to the needle punctures. Patients may notice blood in their urine, stool, or semen. This is generally minimal and should subside within a few days. If bleeding persists or becomes excessive, seeking medical advice promptly is crucial.
4. Rest and Recovery: Rest is essential in the immediate aftermath of the biopsy. While individuals can usually resume light activities within a day or two, strenuous physical activities should be avoided for a short period to allow the body to heal.
5. Hydration: Staying hydrated is essential to flush out residual medications and promote healing. Drinking plenty of water can also help alleviate any discomfort during urination.
6. Follow Post-Biopsy Care Instructions: Healthcare providers will provide specific post-biopsy care instructions. This may include guidelines on personal hygiene, avoiding certain activities, and taking prescribed medications. Adhering to these instructions is crucial for a successful recovery.
7. Monitor for Signs of Infection: Although the risk of infection is minimized with the transperineal approach, it’s essential to monitor for any signs of infection. Symptoms such as fever, increased pain, or unusual discharge should be promptly reported to healthcare professionals.
8. Urinary Symptoms: Temporary urinary symptoms may occur, such as a slow stream or discomfort during urination. These usually resolve independently, but persistent or severe symptoms should be discussed with the healthcare team.
9. Scheduled Follow-Up: Healthcare providers typically schedule a follow-up appointment to discuss biopsy results and address any concerns or lingering symptoms. This is an opportunity for patients to seek clarification on results and discuss any ongoing discomfort.
Individuals need to communicate openly with their healthcare providers during the post-biopsy period. Any unexpected symptoms or concerns should be promptly addressed to ensure a comprehensive and supportive recovery process. While discomfort and minor side effects are joint, most individuals recover fully and resume their regular activities quickly.
6. What is transrectal prostate biopsy?

A transrectal prostate biopsy is a diagnostic procedure where a biopsy needle is inserted through the rectum to collect tissue samples from the prostate gland. This standard procedure helps assess prostate health, detect abnormalities, and diagnose conditions such as prostate cancer.
7. Comparing Transrectal vs. Transperineal Prostate Biopsy
Transrectal and transperineal prostate biopsies are methods for assessing prostate health. The key difference lies in the access point. Transrectal biopsy uses the rectum, posing a higher infection risk. In contrast, transperineal biopsy, through the perineum, offers lower infection risk and enhanced accuracy and is especially suitable for repeat biopsies. The choice depends on factors like patient preference, health conditions, and the need for precision.
8. Which is Better Transrectal or Transperineal Prostate Biopsy
Transperineal prostate biopsy offers several advantages over transrectal biopsy. It minimizes infection risk by avoiding the rectum, enhances accuracy in tissue sampling, and is adaptable for repeat biopsies. The procedure’s lower risk of complications and improved patient comfort make transperineal biopsy a favorable choice, especially in cases where infection prevention and precision are paramount. Consulting with healthcare professionals helps determine the best approach based on individual health and preferences.
9. Research and Expert Opinion on Transperineal Prostate Biopsy

When it comes to transperineal prostate biopsy, the consensus among medical professionals is resounding. Doctors emphasize its effectiveness in obtaining accurate diagnostic information with lower infection risks than transrectal biopsy. These perspectives are reinforced by research findings, consistently supporting the use of transperineal biopsy for its precision and safety. As experts in the field weigh in, the advantages of this approach become increasingly apparent, contributing to its growing recognition in prostate health diagnostics.
10. Future Trends in Prostate Biopsy
The landscape of prostate biopsy is evolving with promising future trends. Emerging technologies and techniques show potential for enhancing diagnostic precision and patient experience. Innovations like advanced imaging modalities, artificial intelligence applications in biopsy planning, and minimally invasive approaches are gaining traction. As research continues, these trends promise to improve the accuracy, efficiency, and overall effectiveness of prostate biopsy procedures, paving the way for future personalized and patient-friendly diagnostic pathways. Stay tuned for groundbreaking developments in the field of prostate health.
What is the ICD-10 code for prostate cancer?
The ICD-10 code for prostate cancer is C61. This alphanumeric code is used for classifying and documenting cases of prostate cancer in medical records, aiding healthcare professionals in accurate diagnosis, treatment, and statistical reporting.
Conclusion
In conclusion, transperineal prostate biopsy stands as a modern, effective, and patient-friendly diagnostic tool. Embracing advancements in urological procedures is a step toward proactive prostate health. Always consult with healthcare professionals for personalized advice tailored to your unique circumstances.
Frequently Asked Questions:
1. What is transperineal prostate biopsy cpt code?
The Current Procedural Terminology (CPT) code for a transperineal prostate biopsy is 55706. This code is used to bill and document the specific procedure of collecting tissue samples from the prostate through the perineum.
2. How long does a transperineal prostate biopsy take?
The duration of a transperineal prostate biopsy varies, but on average, the procedure typically takes about 20 to 30 minutes. Factors influencing the time include the complexity of the case, the number of samples taken, and the patient’s specific anatomy.
3. Transperineal prostate biopsy recovery time?
The recovery time for a transperineal prostate biopsy is relatively short. Most individuals can resume their normal activities within a day or two after the procedure.
4. Cost of a transperineal prostate biopsy?
The cost of a transperineal prostate biopsy can vary based on several factors, including the healthcare provider, geographical location, and any additional services or tests performed during the procedure.
5. Is transperineal biopsy painful?
While individual experiences may vary, a transperineal prostate biopsy is often associated with some discomfort, but it is typically well-tolerated with the use of local or general anesthesia.

